BLOG
Home / Blog
Painful Periods – Are they always normal?

DR ALPHY S PUTHIYIDOM 17 June 2023

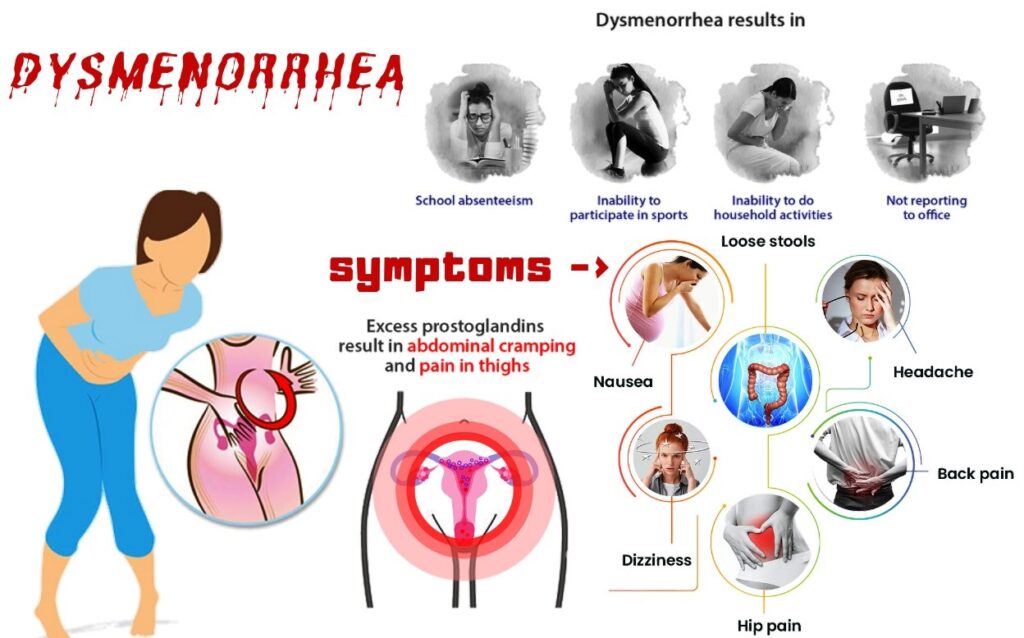
Pain associated with menstruation is called Dysmenorrhea. Many women experience discomfort at the time of their periods. For most, this does not interfere with their daily lives or requires any special attention.
However, for some women their monthly period is painful, problematic and in some cases disabling. It can interfere with their lives because of the pain and inconvenience caused.
How common Is Dysmenorrhea
Dysmenorrhea seems to be the most common gynecological condition in women regardless of age and nationality .The prevalence of dysmenorrhea (painful menstrual cramps of uterine origin) is difficult to determine because of the difference in the severity of the condition—prevalence estimates vary from 45% to 90%.Absenteeism from work and school as a result of dysmenorrhea is common (13% to 51% women have been absent at least once and 5% to 14% are often absent owing to the severity of symptoms).
What causes period pain?
Period pain occurs when the muscular wall of the womb tightens (contracts). Mild contractions continually pass through your womb, but they’re usually so mild that most women can’t feel them.
During your period, the wall of the womb starts to contract more vigorously to encourage the womb lining to shed away as part of your monthly period.
During endometrial sloughing, endometrial cells release prostaglandins as menstruation begins. Prostaglandins stimulates the muscular wall of the womb to contract this contraction compresses the blood vessels lining the womb. This temporarily cuts off the blood supply – and hence oxygen supply – to your womb. Without oxygen, the tissues in your womb release chemicals that trigger pain.
Women with more severe dysmenorrhoea have higher levels of prostaglandins in menstrual fluid and these levels are highest during the first two days of menstruation. It’s not known why some women experience more period pain than others. It may be that some women have a build-up of prostaglandins, which means they experience stronger contractions.
The prostaglandin release may also be responsible for the symptoms of diarrhea, nausea, headache and light-headedness which may occur in association with dysmenorrhea.
Types of Dysmenorrhea?
Dysmenorrhea is broadly thought to be 2 types – Primary or Secondary dysmenorrhea.
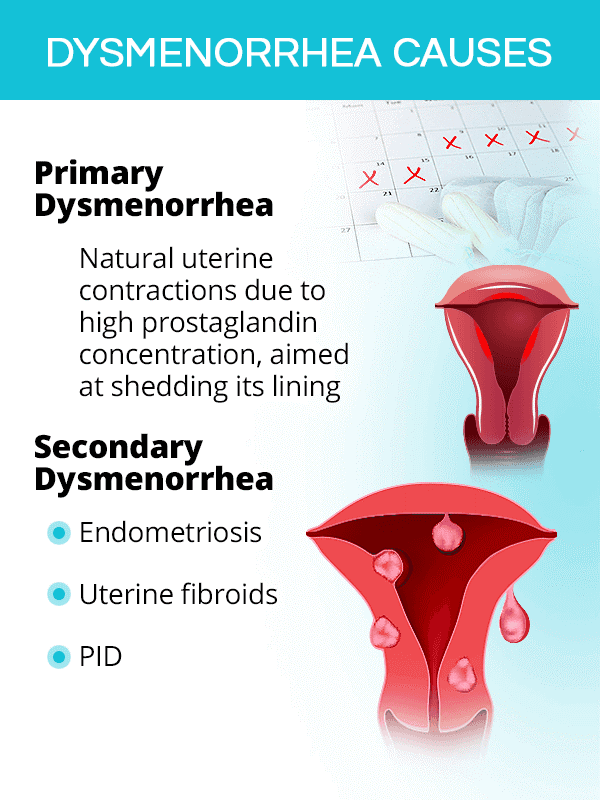
What Causes primary dysmenorrhoea?
Primary dysmenorrhoea occurs in young females with no pelvic pathology.
It often begins with the onset of ovulatory cycles six months to one year after the menarche.
- The pain begins with the onset of the period and may last for 24-72 hours.
- Primary dysmenorrhoea often improves in the third decade of a woman’s reproductive life and after childbirth.
In primary dysmenorrhoea, the uterus works harder than normal to dislodge its lining and the resulting contractions and associated ischaemia (reduced blood flow) cause pain.
Women with primary dysmenorrhoea tend to have raised levels of prostaglandins, which cause more intense contractions of the uterus than normal. The reason for the increased prostaglandins is not known.
Secondary Dysmenorrhoea and Conditions associated with it ?
Secondary dysmenorrhoea occurs in association with some form of pelvic pathology:
It is more likely to occur years after onset of menstruation. The pain can precede the start of the period by several days and may last throughout the period. There may be associated dyspareunia.
Secondary dysmenorrhoea may occur as a result of:
- Endometriosis–where cells that normally line the womb start to grow in other places, such as in the fallopian tubes and ovaries; these cells can cause intense pain when they shed and fall away
- Fibroids–non-cancerous tumors that can grow in the womb and can make your periods heavy and painful.
- Pelvic inflammatory disease– where your womb, fallopian tubes and ovaries become infected with bacteria, causing them to become severely inflamed.
- Adenomyosis – where the tissue that normally lines the womb starts to grow within the muscular womb wall, making your periods particularly painful.
- Developmental abnormalities.
- The copper-containing intrauterine contraception device (Cu-IUCD) may cause pelvic pain in the first few months after fitting but does not influence the severity of dysmenorrhoea in the longer term.
Can period pain affect fertility?
Period pain that’s part of normal menstrual cycle won’t affect fertility. However, if the cause is an underlying condition, this may affect fertility.
For example, endometriosis and pelvic inflammatory disease can cause scarring and a build-up of tissue in your fallopian tubes, making it harder for sperm to reach and fertilise an egg.
Fibroids and adenomyosis can affect the womb and cause pain and heavy menstrual bleeding which can affect conception.
Treatment options for Dysmenorrhoea
Women with dysmenorrhoea need a thorough medical examination to make sure their period pain is not caused by certain reproductive disorders such as endometriosis or fibroids.

Treatment options for Dysmenorrhoea
Treatment options can include:
- Pain-relieving medication, such as paracetamol .Medication that inhibits prostaglandins, such as ibuprofen or other anti-inflammatory medication
- Regular exercise and attention to overall physical fitness
- Avoid Smoking .
- If the woman with dysmenorrhoea does not wish to conceive, offer her hormonal contraception. Ovarian suppression appears to control cyclical pelvic pain, whether or not caused by endometriosis. Adolescents and young adults who do not respond to hormonal treatment after three months should be evaluated for secondary causes of dysmenorrhoea.This is likely in approximately 10% of patients.
- In Case of secondary dysmenorrhoea the underlying pathology should be identified and treated . Patients with Endometriosis , Fibroid and adenomyosis where medical management fails may require appropriate surgical treatment . Even though painful periods is a common problem If pains are more than an inconvenience, it’s wise to consult a gynecologist.

Dr. Alphy S Puthiyidom
MBBS, MD(Obs&Gn),FMIS(Laparoscopy)
Head of the Department Obstetrics & Gynecology
Advanced Gynecological Laparoscopic Surgeon
& Pelvic Reconstructive Surgeon
MEDICLINIC WELCARE HOSPITAL
Al Garhoud, Dubai
MEDICLINIC PARKVIEW HOSPITAL
Umm Sequim, Al Barsha South 3, Dubai
Appointments 800-1999