Hysteroscopy
This article outlines the common reasons doctors advise this investigation, how a hysteroscopy is carried out, potential risks as well as benefits, and what to expect afterwards.
What is hysteroscopy?
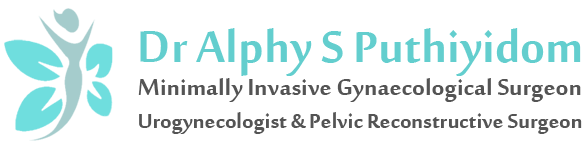
Hysteroscopy is a simple investigation that involves looking into the uterus (womb) with a telescope called a hysteroscope.
Why is hysteroscopy performed?
Hysteroscopy is a procedure used to investigate abnormal vaginal bleeding, such as bleeding after the menopause, heavy periods, and bleeding between periods.
It is also used when abnormalities of the uterus are found during an ultrasound scan.
These include:
• Thickening of the lining of the uterus known as the endometrium.
• Polyps (fleshy tissue protruding from the endometrium).
• Fibroids (swellings that arise from the muscle of the uterus).
• As part of investigations of recurrent miscarriage if an abnormality of the womb is suspected.
• As part of investigations of infertility
How is hysteroscopy carried out?
The hysteroscope is very narrow and is passed through the cervix into the cavity of the uterus. As the uterus is usually ‘folded up’, a saline fluid is introduced to ‘open up the womb’ so that the doctor can have a clear and direct view of the inside of the womb. Sometimes the cervix needs to be dilated using special dilating instruments to allow the hysteroscope to pass through.
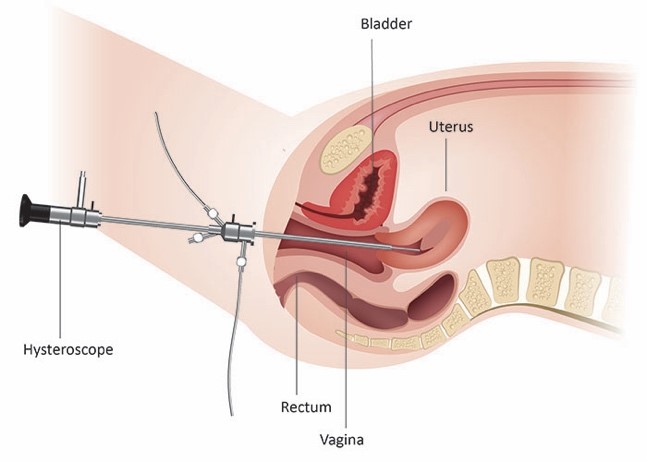
Small polyps, fleshy tissue that protrudes (sticks out) from the lining of the womb, can be removed during a hysteroscopy.
Fibroids can also be removed, if they protrude into the cavity of the uterus, using a special hysteroscope with an electrical loop, known as a resectoscope or with an intrauterine shaver.
Are there risks with this procedure?
Hysteroscopy is usually a simple procedure without significant risks. However, there are risks with any surgical procedure. If the hysteroscopy involves a surgical procedure such as removal of a fibroid, the risks are increased.
The risks and complications are:
• Perforation of the wall of the womb which could necessitate a laparoscopy and repair – incidence approximately less than 2%.
• Infection requiring antibiotics – incidence less than 2%.
• Bleeding requiring blood transfusion – rare unless a large fibroid is being removed.
• Anesthesia risks – these are very uncommon.
How long does the procedure take and how long will I be in hospital?
The procedure should take no more than about 20-60minutes. If this procedure is carried out with a general anaesthetic (when you are asleep) it will be as a day case procedure, and therefore you will only be in hospital for approximately half a day.
What should I expect after the procedure?

• You will stay in the recovery room within the theatre suite after the operation while you wake up from your anaesthetic. You will then be transferred in your bed to the Day Procedure Unit.
• During your recovery your nurse will take frequent observations of your vital signs (e.g., temperature, pulse, blood pressure) for several hours after the surgery. As you become fully recovered, these observations become less frequent but remain regular until you leave hospital later the same day.
• You will be given pain relief as needed.
• Your nurse will discuss your follow-up appointment and any discharge arrangements that have been made with you.
• You should be eating and drinking normally and be mobilizing.
Discharge advice

If you had general anesthesia, you would need to rest until the effects of the anesthesia have passed. You will need to arrange for someone to drive you home. You should try to have a friend or relative stay with you for the first 24 hours.
• do not consume alcohol for the remainder of the day
• do not drive a car, motorbike, or ride a bicycle
• do not sign any legal documents or make any important decisions
• do not engage in sports or heavy lifting.
• You may have light, menstrual type bleeding for a few days.
• There may some menstrual like cramps for 1-2 days. Paracetamol should be sufficient to control the discomfort.
The bleeding is usually mild and should settle within seven days.
To reduce the risk of infection whilst you are bleeding you should:
• Use sanitary pads rather than tampons.
• Not have vaginal sex for one week after and until you stop bleeding.
• Avoid swimming for two weeks.
• Take it easy for the first one or two days and take painkillers as needed.
• You should be able to return to work the following day but may require more time off work depending on the procedure performed.
What about the results and follow up?
A discharge summary mentioning the details of the procedure will normally be given to you before you leave hospital. Follow-up will be after 10-14 days; it is mainly to discuss on the test result on the tissue sample sent from the procedure.
When you get home
If during the next five days you experience any of the following, please visit your Gynecologist or hospital Emergency department.
• A smelly vaginal discharge
• Heavy prolonged bleeding
• Abdominal cramps that are not controlled with painkillers.
• High temperature (fever) of 38 degrees or above
• Feeling generally unwell
• Unable to empty your bladder or bowel
• Very fast heart rate.
Why is it important to choose a specialized minimally invasive gynecological surgeon for hysteroscopy?
Invariably, all Ob-Gyns are trained in doing hysteroscopic procedures as they are mostly not a complicated procedure. You need to find an experienced hysteroscopic surgeon, especially if you are undergoing hysteroscopic surgery for infertility-related issues. The experience of the surgeon matters a lot as the successful outcome depends on that.