BLOG
Home / Blog
Can Endometriosis be prevented? From Awareness to Action!

DR ALPHY S PUTHIYIDOM 23 August 2023
Can Endometriosis be prevented? From Awareness to Action!
Disease Prevention: What Does It Mean?
The prevention of a disease refers to the various measures and actions taken to avert or minimize the occurrence of illnesses and associated health damages. These measures aim to reduce the risks linked to a particular disease or delay its onset. Depending on when these preventive measures are employed, they are categorized into primary, secondary, or tertiary prevention.
- Primary prevention focuses on averting the onset of diseases. For instance, one way to prevent type II diabetes or heart attacks is by adopting a healthy lifestyle that includes nutritious eating habits, physical activities, and overall wellness practices. Another example is vaccination, which safeguards against influenza and other infectious diseases. Primary prevention necessitates understanding the reasons behind the disease's occurrence, enabling the treatment of underlying causes before the disease manifests.
- Secondary prevention entails early detection of a developing disease. Screening programs for cervical cancer, breast cancer, or colorectal cancer are examples of secondary prevention. These programs enable the early diagnosis of invasive lesions, facilitating prompt treatment and preventing the progression of the disease.
- Tertiary prevention focuses on mitigating the consequences of a disease, preventing its recurrence, and minimizing the exacerbation of an ongoing condition. It involves interventions that help alleviate the sequelae of a disease that has already occurred, aiming to improve the patient's quality of life and prevent further complications.
In this blog, we will explore the possibility of preventing endometriosis.
Primary prevention of endometriosis
In order to fully understand the prevention of endometriosis, it is crucial to delve into the reasons behind its occurrence. The development and underlying causes of this condition are complex, and several ideas have been put out to explain them.
Some commonly suggested theories include the implantation theory, coelomic metaplasia theory, and the concept of tissue injury and repair. However, none of these theories can provide a comprehensive explanation for the entire process of endometriosis development. Currently, researchers rely on a combination of these theories, along with genetic defects, epigenetic phenomena, and other influencing factors, to gain insights into the pathogenesis of this condition.
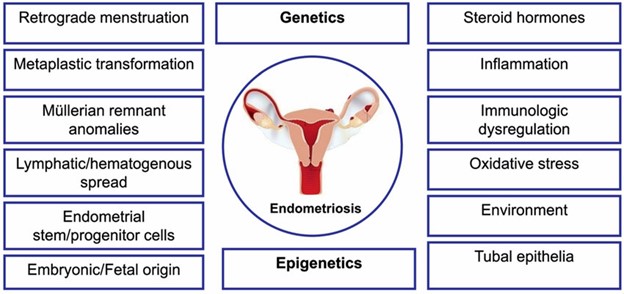
Several factors play a significant role in endometriosis, such as hyperperistalsis, hyperestrogenism, inflammatory and immunological processes, prostaglandin biosynthesis, angiogenesis, oxidative stress, and more. Researchers have studied various potential risk factors, including menstrual cycle length, menstruation duration, pregnancy history, and miscarriages. However, data on other factors like age at menarche, oral contraceptive use, BMI, smoking, caffeine consumption, nutrition, and physical activity is inconclusive or conflicting.
Furthermore, some things in the environment, such as polychlorinated biphenyls (PCBs), bisphenol A (BPA), and phthalates, have been linked to changes in our genes and inflammation in our bodies. These substances, which are found in various products and materials, can potentially cause alterations in our genetic material and trigger processes that lead to inflammation. It is important to be aware of these environmental factors and take steps to minimize exposure to them in order to protect our health.
In summary, the exact cause of endometriosis remains unclear, and no causal therapy or primary preventive measures have been established. The potential preventive measures that have been proposed are either impractical or lack sufficient evidence of effectiveness.
In conclusion, primary prevention of endometriosis is currently not feasible due to the lack of clear understanding regarding its etiology.
Secondary Prevention of Endometriosis
Secondary prevention focuses on achieving early diagnosis of a disease. Effective diagnostic measures are already available and accessible to a significant portion of the global population. However, even in developed countries, the time taken to receive a diagnosis is often reported to be around 8 to 10 years from the onset of symptoms. To enable early diagnosis, it is crucial to increase awareness about the disease among both the general population and the medical community.
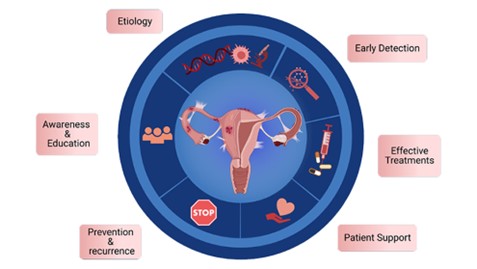
Implementing effective educational programs for the general population, starting from school-age, has shown positive outcomes in raising awareness about endometriosis. Events such as Endometriosis Awareness Month have already played a significant role in increasing awareness and understanding of the disease. It is crucial to extend education efforts to pediatricians and general practitioners who may not have as much familiarity with endometriosis as gynecologists but often serve as the first point of contact for patients. These healthcare professionals should be equipped with knowledge about endometriosis to ensure early detection and appropriate referrals to gynecologists who specialize in this area. Moreover, educational programs targeting gynecologists should aim to provide detailed information about the disease and emphasize the importance of referring suspected cases to specialized gynecologists with expertise in endometriosis.
Optimizing the diagnostic workup is essential for achieving early diagnosis of endometriosis. Specific endometriosis questionnaires can be utilized as a first step in the diagnostic process. Gynecological examinations, transvaginal or transrectal ultrasounds are commonly used as initial diagnostic measures. In cases where further confirmation is required, MRI or laparoscopy may be recommended. While salivary mRNA is a newer modality for detecting endometriosis, its availability is currently limited.
Tertiary Prevention of Endometriosis
Tertiary prevention is used to help improve the outcome of endometriosis, prevent it from coming back, and stop it from getting worse. To achieve this, medical or surgical treatments can be used. These treatments are generally effective in preventing the progression of the disease and the development of long-term problems like infertility and chronic pain. Hormonal treatments, like progestogens and combined oral contraceptives, can be considered as a form of tertiary prevention if they can stop menstrual periods. However, it’s important to use these treatments consistently and without interruptions for them to be effective in the long run.
Systemic hormonal treatment options which can be used also as a preventive treatment after surgical removal of endometriosis include oral progestogens such as dienogest and combined oral contraceptives (COC). These measures lead to hypoestrogenism by influencing the hypothalamic hypophysical axis causing decrease in proliferation, reduction of lesion size and activity.
These effects can also be achieved by GnRH analogue treatment. As these substances can cause menopausal symptoms and lead to osteoporosis in case of long-term treatment they are of limited value as a potential preventive treatment. There is data on postoperative use. A 6-month treatment using GnRH analogues led to a reduction of risk of recurrence. GnRH analogues better should be administered together with an add back therapy. Add back therapy leads to elevation of estrogen levels resulting in decrease of hypoestrogenic side effects without compromising effectiveness of GnRH analogue treatment.
A recent study confirmed that hormonal therapy, in its various forms, is effective in preventing the recurrence of endometriosis. Local hormonal treatments, such as progestogen-releasing intrauterine devices (IUDs), can also be used to shrink the endometrial tissue and reduce the risk of recurrence. Levonorgestrel-releasing IUDs have been shown to be effective in delaying the disease from coming back.
Surgical removal of endometriosis is another form of tertiary prevention. It can lead to a reduction or elimination of symptoms and prevent complications like bowel obstruction(blockage of the bowel ) or as hydronephrosis (swelling of the kidneys). During surgery, the goal is to remove all visible endometriosis lesions while considering the patient’s quality of life. Sometimes compromises need to be made if removing all lesions would negatively impact the patient’s quality of life. For ovarian endometriotic cysts, cystectomy is the preferred surgical option to reduce the chance of the disease recurring.
Conclusion:
- Primary prevention of endometriosis is not currently feasible.
- Secondary prevention can be achieved through educational programs for healthcare professionals and the general population, as well as by improving diagnostic processes.
- Empowering general obstetricians and gynecologists with comprehensive training in endometriosis diagnosis, while highlighting the crucial significance of referring suspected cases to specialized gynecologists proficient in endometriosis care.
- Complete resection of symptomatic lesions, especially in cases of deep infiltrating endometriosis, leads to tertiary prevention by halting disease progression and preventing complications.
- Tertiary prevention involves postoperative continuous hormonal therapy, with progestogen-only therapy as the preferred choice.
- Combined oral contraceptives (COCs) are effective in preventing recurrence, particularly for endometriotic ovarian cysts.
References
Koninckx PR, Ussia A, Adamyan L, Wattiez A, Gomel V, Martin DC. Pathogenesis of endometriosis: the genetic/epigenetic theory. Fertil Steril. 2019
Hirsch M, Begum MR, Paniz E, Barker C, Davis CJ, Duffy J. Diagnosis and management of endometriosis: a systematic review of international and national guidelines. BJOG. 2018
Zakhari A, Delpero E, McKeown S, Tomlinson G, Bougie O, Murji A. Endometriosis recurrence following post-operative hormonal suppression: a systematic review and meta-analysis. Hum Reprod Update. 2020
https://www.eshre.eu/Guideline/Endometriosis 2022

Dr. Alphy S Puthiyidom
MBBS, MD(Obs&Gn),FMIS(Laparoscopy)
Head of the Department Obstetrics & Gynecology
Advanced Gynecological Laparoscopic Surgeon
& Pelvic Reconstructive Surgeon
MEDICLINIC WELCARE HOSPITAL
Al Garhoud, Dubai
MEDICLINIC PARKVIEW HOSPITAL
Umm Sequim, Al Barsha South 3, Dubai
Appointments 800-1999