BLOG
Home / Blog
Stress Urinary Incontinence in women

DR ALPHY S PUTHIYIDOM 17 June 2023
What is Stress Urinary Incontinence?

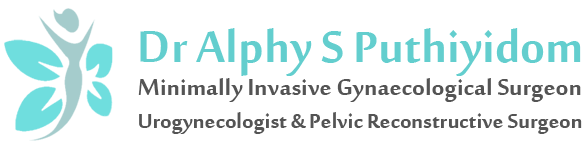
Stress Urinary Incontinence (SUI) is the involuntary leakage of urine during activities such as coughing, sneezing, lifting, laughing or exercising. SUI affects at least 15-20% of women, many of whom do not realize that there are simple, effective treatment options available.
What Causes Stress Urinary Incontinence?
The urethra and bladder are supported by the pelvic floor muscles, which contract during coughing, sneezing and exercise to prevent leakage. Weakness in the muscles or damage to the bladder neck support can result in leakage.
Causes of Stress Urinary Incontinence
- Pregnancy and vaginal birth.
- Obesity, chronic cough, chronic heavy lifting and constipation. These can cause an increase in abdominal pressure and aggravate stress incontinence.
- Genetically inherited factors.
What investigations may be performed to diagnose Stress urinary incontinence?
- To help with diagnosis, your doctor may ask you to cough while you have a comfortably full bladder.
- You may be asked to fill in a frequency volume chart (bladder diary), recording how much you drink, as well as the number of times you pass urine and the volume passed each time. A record of the amount of leakage is also kept.
- Your doctor may recommend urodynamic studies. Urodynamic investigate the bladder’s ability to fill and empty, and the mechanism or cause of the incontinence.
- An ultrasound scan may be used to determine how much urine is left in the bladder after it empties and can identify if there are any other causes for your symptoms.
- A urine test may be performed to look for a urinary tract infection.
All these tests are designed to help plan the best treatment for each individual.
What are the treatment options for Stress Urinary Incontinence?
Your physician will advise you on the best options for you, but initially you may be recommended conservative treatment.
- General lifestyle changes. Aim to drink enough to pass urine 4 to 6 times per day (usually about 1.5-2 liters; half a gallon). Maintaining weight within a healthy range has been shown to reduce the severity of SUI problems. Avoiding causes of constipation and cutting out smoking can also help.
- Pelvic floor exercises. Pelvic Floor exercises (PFE) can be a very effective way of improving symptoms of SUI. Like all training, the benefits of pelvic floor exercises are maximized if practice is carried out regularly over a period of time. Maximum benefit usually occurs after 3 to 6 months of regular exercising. You may be referred to a therapist who specializes in teaching PFEs to supervise this

- Continence devices. Continence devices are available which fit in the vagina and help control leakage. These can be inserted prior to exercise or in the case of a vaginal pessary, worn continuously. These types of devices are most suitable for women with minor degrees of urinary incontinence or who are waiting definitive surgical treatment.
Surgical treatment options for Stress urinary Incontinence
The aim of surgery is to correct weakness of the supports of the bladder neck. Many surgeons would want to avoid surgery until a woman’s family is complete because future pregnancy may compromise the results of the initial surgery.
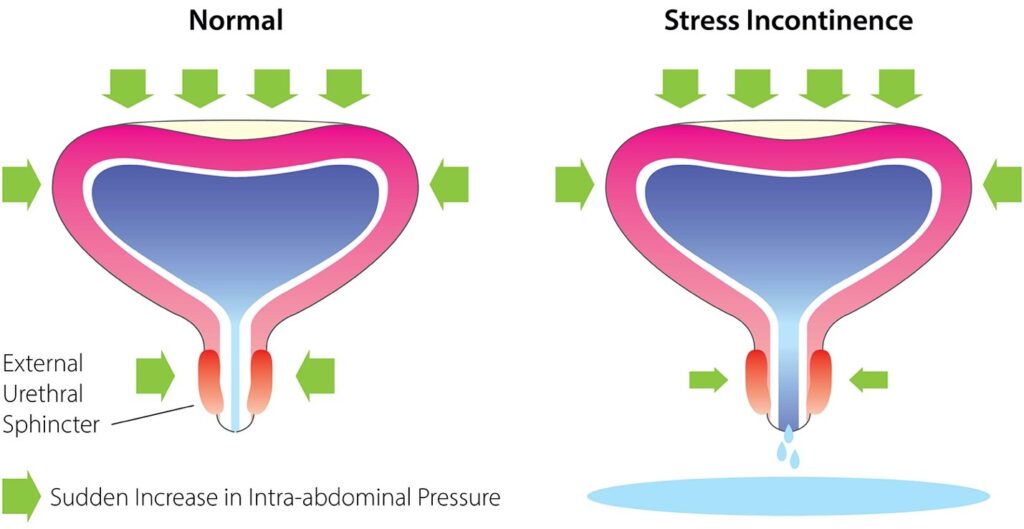
- Mid-urethral sling procedures. Before 1993, the treatment of stress incontinence often involved major surgery with an abdominal incision. The most common treatment now involves the use of a permanent sling that lies under the middle section of the urethra. The sling works by providing support to the urethra when you cough, sneeze or exercise. Following a small incision in the vagina, the sling can be put into position in several ways.
- TVT -Retro pubic slings: pass under the urethra, then run behind the pubic bone with the tape exiting out through two small cuts just above the pubic bone.
- TOT-Trans obturator slings run under the mid part of the urethra and pass out through 2 incisions in the groin. 80-90% of women undergoing retro pubic or Trans obturator sling procedures are cured or improved of their stress incontinence symptoms following surgery.
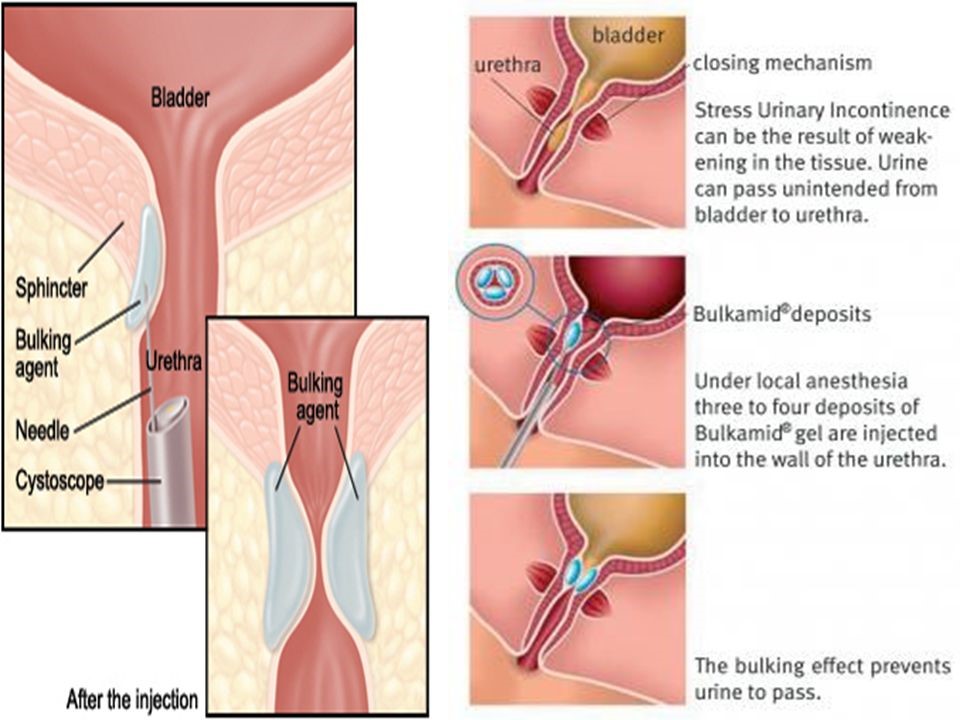
- Bulking agents: Substances can be injected around the bladder neck and into the urethral sphincter to bulk it up and reduce the caliber of the urethra. An anesthetic may be required for the operation, but many are performed under local anesthetic only. Some burning or stinging when urinating, after the operation, is quite common. Sometimes injections need to be repeated. Success rate is less than sling surgeries
- Laparoscopic Burch (colposuspension) – The surgery involves the passage of 4-6 permanent sutures that suspend the vaginal tissue underlying the bladder to the back of the pubic bone in order to support the bladder neck and urethra and restore continence. This is not very commonly performed, reserved in cases were other methods fail. This operation is not designed to cure urge incontinence/overactive bladder (OAB) symptoms, although up to 50% of women notice some improvement in OAB symptoms following sling surgery. However, in a small percentage of women with OAB, their symptoms may worsen. Female Urinary incontinence is a very common problem. There is good evidence to suggest that it might take up to 5 years before a woman seeks help and the main reasons cited was that it was deemed to be part of aging and women are embarrassed to talk about this. Stress urinary incontinence is a condition which can be easily treated.

Dr. Alphy S Puthiyidom
MBBS, MD(Obs&Gn),FMIS(Laparoscopy)
Head of the Department Obstetrics & Gynecology
Advanced Gynecological Laparoscopic Surgeon
& Pelvic Reconstructive Surgeon
MEDICLINIC WELCARE HOSPITAL
Al Garhoud, Dubai
MEDICLINIC PARKVIEW HOSPITAL
Umm Sequim, Al Barsha South 3, Dubai
Appointments 800-1999