BLOG
Home / Blog
Pelvic Organ Prolapse: What Women Needs to Know

DR ALPHY S PUTHIYIDOM 17 June 2023

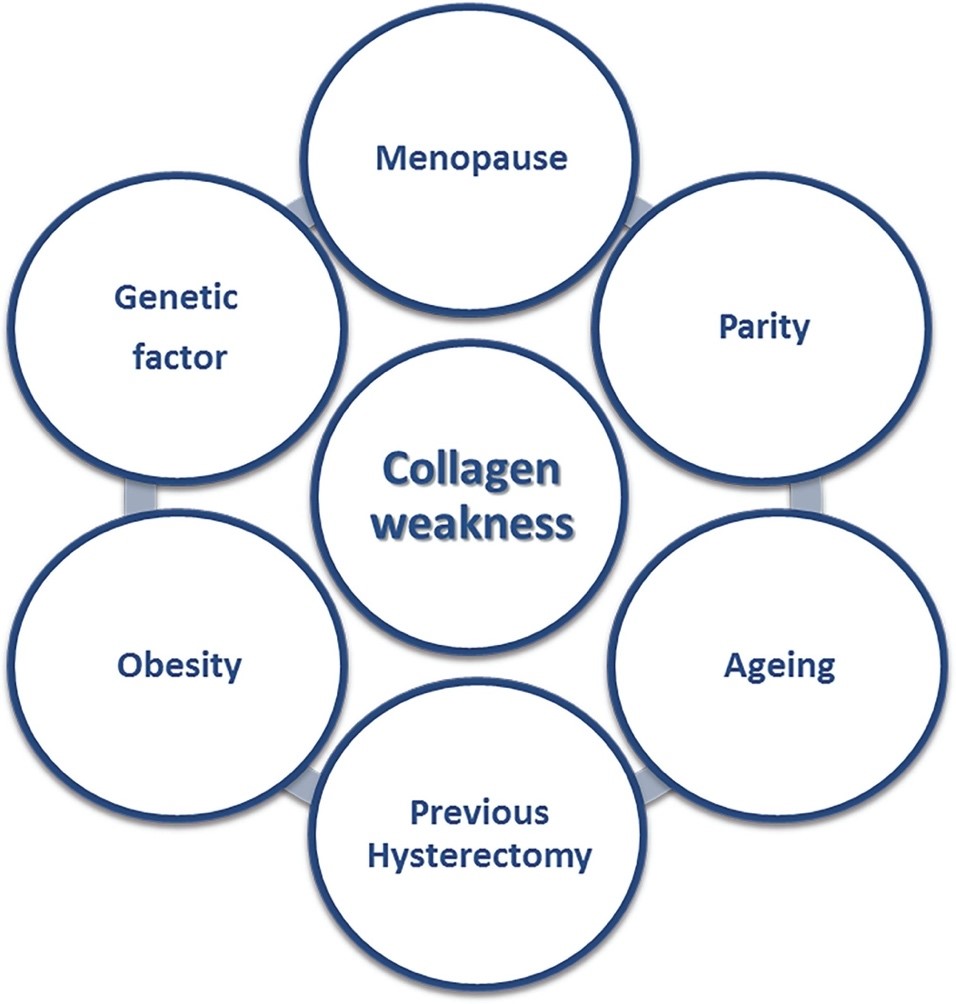
Genital prolapse is a distressing condition and a large percentage of women develop some form of vaginal prolapse during their lifetime, most commonly following menopause, childbirth, or a hysterectomy. Most women who develop this condition are older than 40 years of age.
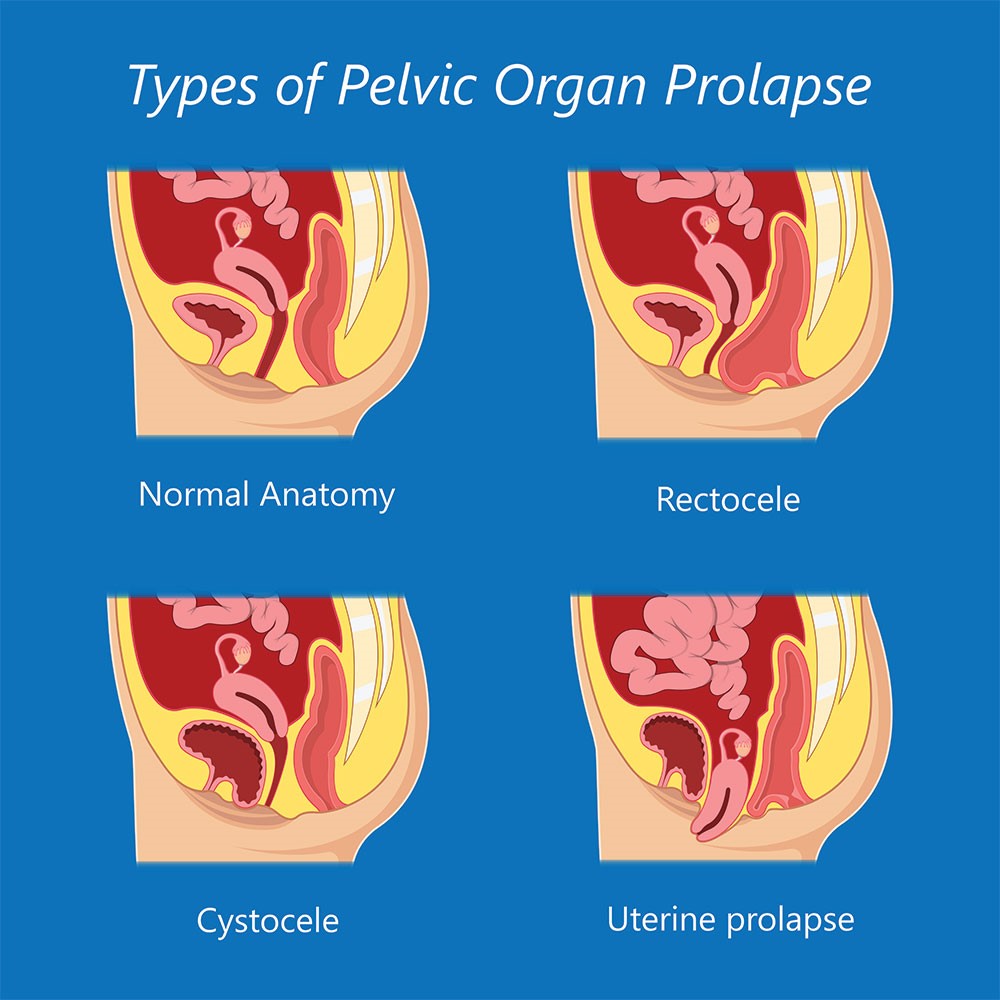
Pelvic organ prolapse is descent of the pelvic organs (Urinary bladder, uterus (womb) and rectum) into the vagina, often accompanied by urinary, bowel, sexual, or local pelvic symptoms. The incidence of genital prolapse is difficult to determine, as many women do not seek medical advice. It has been estimated that a half of parous women lose pelvic floor support, resulting in some degree of prolapse, and that of these women 10-20% seek medical care.
What causes a Genital prolapse?
Prolapse tends to run in families. It is more likely after menopause. Estrogen is the hormone that helps to keep the muscles and tissues of the pelvic support structures strong. After menopause, the estrogen level declines; and the support structures may weaken leading to prolapse.
Childbirth is another main cause of prolapse. On the way down the vagina, the baby can stretch and tear the supporting tissues and pelvic floor muscles. The more vaginal births you have, the more likely you are to have a prolapse.
About half of all women who have had a child have some level of prolapse, but only one in five women need to seek medical help.
- Prolapse can also happen in women who haven’t had a baby, mainly if they cough, strain on the toilet, or lift heavy loads.
- Prolapse can also happen in women who have had their womb removed (that is, had a hysterectomy). In a case like this, the top of the vagina (the vault) can prolapse.
What are the signs and symptoms of having Genital prolapse?
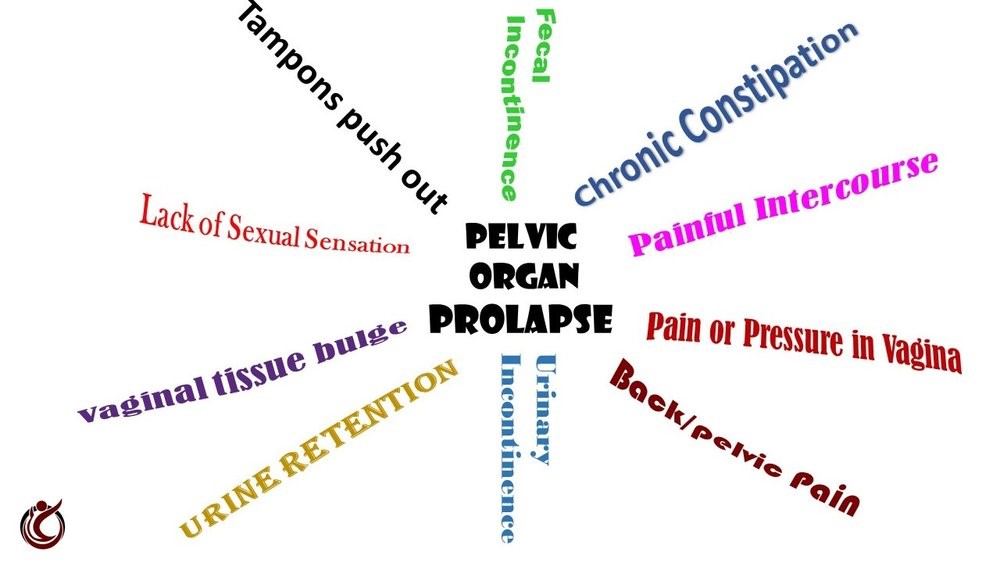
Many women who have pelvic organ prolapse don’t have symptoms. When women do experience symptoms, they can range from relatively minor to debilitating. The signs of genital prolapse depends on the type, severity of prolapse and how much pelvic organ support has been lost. Early on, you may not know you have a prolapse as there will be no symptoms, but your doctor or nurse might be able to see you prolapse when you have your routine Pap smear test.
When a prolapse is further down, you may notice things such as:
- a heavy sensation or dragging in the vagina
- something ‘coming down’ or a lump in the vagina
- a lump bulging out of your vagina, which you see or feel when you are in the shower or having a bath
- sexual problems of pain or less sensation
- your bladder might not empty as it should, or your urine stream might be weak
- urinary tract infections might be reoccurring, or
- it might be hard for you to empty your bowel.
These signs can be worse at the end of the day and may feel better after lying down. If the prolapse bulges right outside your body, you may feel sore and bleed as the prolapse rubs on your underwear.
What can be done to treat prolapse once it has happened?
Prolapse can be dealt in many ways depending on the symptoms and the severity.
The simple approaches
Prolapse can often be treated without surgery, chiefly in the early stages, and when the prolapse is mild and when patient does not have much symptoms. The simple approach can mean:
- Pelvic floor muscle training, where a program of treatment is planned to suit your individual needs, with the advice of a pelvic floor physiotherapist.
- Learning what caused your prolapse, and making needed lifestyle changes, such as improving your diet, fluid intake, exercising and losing weight
- Being aware of good bowel and bladder habits to avoid straining on the toilet.
Treatments, like lifestyle changes and physical therapy, are considered more conservative in approach and so are generally tried first. Pessaries, a device inserted into the vagina to provide support to the pelvic floor, offer a temporary solution to pregnant women or, in some cases, a permanent solution to women who are not medically fit for surgery.
Laser treatment for vaginal relaxation
Laser treatment is ideal for those women who have vaginal relaxation causing symptoms but not to the extent that they want to submit to a surgical intervention. It is mainly a matter of quality of life. The laser treatment is less effective than surgical intervention not advised in uterine prolapse which is a result of loss of the suspensory mechanism of the uterus which exists within your pelvis, away from the vaginal epithelium.
Laser treatment is recommended in patients having milder form of vaginal prolapse and stress urinary incontinence.
Surgical treatment for prolapse
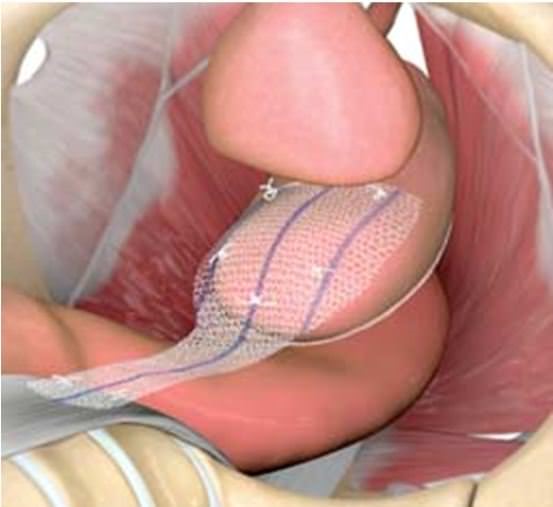
- Surgery can be done to repair torn or stretched support tissues and ligaments. There are different ways to do this surgery including:
- Laparoscopic (keyhole)
- Robotic
- Vaginal approach
The surgery makes the vaginal wall stronger and helps the tissues support the pelvic organs. There different surgical options and choosing one depends upon which organ(s) have descended, a woman’s age, history of previous pelvic surgery, and whether she wishes to retain her uterus. Various minimally invasive surgical approaches are available now in Young patients who wish to retain uterus and want to have pregnancies in future.
What can be done to prevent prolapse?
It is much better to prevent prolapse than try to fix it! If any women in your close family have had a prolapse, you are more at risk.
As prolapse is due to weak pelvic tissues and pelvic floor muscles, all women should keep their pelvic floor muscles strong – no matter what their age. Pelvic floor muscles, just like any other muscles, can be made stronger with the right exercises. It is important to strengthen the pelvic floor muscles after vaginal delivery by regularly performing Kegel’s exercises.Continuing to do Kegel exercises regularly after giving birth not only helps you to prevent prolapse but maintain bladder control, it also improves the muscle tone of your vagina, making sex more enjoyable.
- Women at risk for vaginal prolapse (including those who have had corrective surgery) should, if possible, avoid heavy lifting or any activity that increases pressure within the abdominal cavity.
- Obesity puts extra stress on the muscles and ligaments within the pelvis and vagina. Weight reduction can help prevent this condition from developing or recurring.
When to Seek Medical Care for Prolapsed Vagina
A large percentage of women develop some form of vaginal prolapse during their lifetime. Many women who develop the symptoms of a vaginal prolapse do not seek medical help because of embarrassment or other reasons.
Any woman who experiences symptoms that may indicate a vaginal prolapse should contact her doctor. A vaginal prolapse is rarely a life-threatening condition. However, most prolapses gradually worsen and needs be corrected. Thus, timely medical care is recommended to evaluate for and to prevent problematic symptoms and complications caused by weakening tissue and muscles surrounding the vagina.

Dr. Alphy S Puthiyidom
MBBS, MD(Obs&Gn),FMIS(Laparoscopy)
Head of the Department Obstetrics & Gynecology
Advanced Gynecological Laparoscopic Surgeon
& Pelvic Reconstructive Surgeon
MEDICLINIC WELCARE HOSPITAL
Al Garhoud, Dubai
MEDICLINIC PARKVIEW HOSPITAL
Umm Sequim, Al Barsha South 3, Dubai
Appointments 800-1999